HemCon Chitosan Hemostatic Devices and the Body’s Clotting Cascade
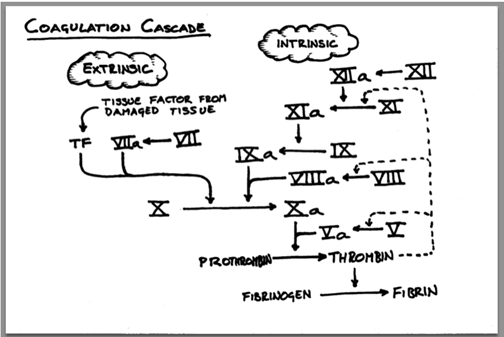
In our final article of our first of many educational series, we are going to review the body’s natural clotting cascade and how HemCon’s hemostatic devices do not rely on this process to control bleeding. We often talk about how our products work “outside of the clotting cascade” but what does that really mean? What is the clotting cascade and why does it matter that HemCon products work outside of it? First, we must understand the clotting cascade. By quickly glancing at the diagram on this page, it will make perfect sense…. Well, perhaps an explanation is necessary. The human body is full of complex processes that are truly amazing, and the clotting cascade is certainly one of them.
Don’t worry about the above diagram. What you need to know is that when you cut yourself and you want the bleeding to stop, or when a physician performs surgery and needs to stop the bleeding post-procedure, there are many things within your bloodstream that need to happen for it to successfully form a clot. In fact, there are 13 “clotting factors,” and each factor has an “inactive” form that gets converted into an “active” form to enable clotting. This conversion is the clotting cascade.
Before we go further, let’s get some common definitions out of the way:
- Clotting Factors – any of several substances in blood plasma that are involved in the clotting process, such as calcium, prothrombin, Fibrogen, and tissue. Each clotting factor is assigned a number 1 through 13.
- Collagen – the main structural protein found in the skin and other connective tissues.
- Prothrombin – a protein in blood plasma that gets converted into thrombin.
- Thrombin – an enzyme in blood plasma which causes the clotting of blood by converting fibrinogen into fibrin.
- Fibrinogen – a soluble protein in blood plasma from which fibrin is produced thanks to the action of thrombin.
- Fibrin – an insoluble protein formed from fibrinogen during the clotting of blood. It forms a “fibrous” mesh that impedes the flow of blood… the clot!
- Platelets – small cells in the blood that help with forming blood clots.
When there is damage to a blood vessel (from an unanticipated cut, or surgical procedure), collagen is exposed to circulating platelets in the blood. These platelets bind directly to collagen and create a platelet plug. This is the first thing that happens, triggering the clotting cascade. We mentioned above that there are 13 factors that need to convert from inactive to active inside the clotting cascade. These 13 factors are organized in what is referred to as pathways, the intrinsic pathway and the extrinsic pathway. The intrinsic pathway is activated when there is direct damage to the blood vessel. The extrinsic pathway is activated by direct damage to the blood vessel as well, but also by many other things such as tissue damage outside of the blood vessel, hypoxia, sepsis, malignancy, and inflammation. Think of these paths as separate roads, each with different factors with conversion processes that ultimately come together at factor 10 to form one road, starting the common pathway. And within the common pathway, the 2 most important factors are thrombin and fibrin.
Fibrin is factor number 1, the protein that forms a mesh, trapping platelets and ultimately creating the clot. But it cannot happen without thrombin, factor number 2, which plays a big role in activating many of the other factors, both within the intrinsic and extrinsic pathways (factors 5,7,8,11 and ultimately 13). Factor 13 is the last and final clotting factor number. When you’ve reached factor 13, your blood has formed a clot!
By now you are an expert at understanding the body’s natural clotting cascade. Maybe not, it can be confusing even for those that are somewhat familiar with it. It is truly amazing that this process takes place every day in all of us when we cut ourselves or have a planned event. And now that you know about it, we can get back to the original question of how the HemCon hemostatic devices work “outside of the clotting cascade,” and why it matters.
If you cut yourself and use a store-bought bandage or piece of gauze, and apply gentle pressure to stop the bleeding, you will need the clotting cascade to kick into gear and allow the process to run its course, ultimately creating a clot (thrombin to fibrinogen to fibrin). Think about all the factors mentioned above! This process works fast in some people, and very slow in others. For patient’s on blood thinners (anti-coagulants) their pace of clotting is slowed by impacting certain factors limiting thrombin’s ability to exercise its power in creating a clot. There are also certain diseases like hemophilia or Von Willebrand disease that hinder the ability of the clotting cascade in affected individuals. The clotting cascade does not always cooperate as it does on paper and charts. Getting the clotting cascade to work could take a very long time in some cases.
This is where “working outside the clotting cascade” comes into play for the HemCon hemostatic devices. Our positively charged chitosan devices simply attract the negatively charged platelets and blood cells to create a strong clot at the wound site, meaning, you do not have to worry about all those factors in the clotting cascade running their course. Of course, they will run their course behind the scenes, but HemCon devices do not rely on them at all. Other hemostatic devices made from other sources work by affecting the extrinsic pathway, speeding up the clotting cascade process, but still must rely on part of the clotting cascade being intact.
The HemCon hemostatic devices have been stopping bleeding since 2001 when first introduced by the U.S. Army to control traumatic bleeding. Being able to “work outside of the clotting cascade” played a large role in their decision to supply HemCon products to U.S. Soldiers.
